质子放疗对儿童脑癌患者的安全性如何?
与手术后提供的传统X射线辐射相比,质子治疗对儿童脑癌患者的安全性如何?
南澳大利亚大学(UniSA)研究人员的一项新研究将在未来两年内探索这个问题,通过对美国一所质子医院的数据对比,根据个别癌症种类、辐射敏感性、儿童的性别和年龄来考核病人的治疗结果进行预测并验证。
南澳大学博士生Mikaela Dell'Oro和她的导师(Michala Short博士、Puthenparampil Wilson博士和Eva Bezak教授)已获得第7频道儿童研究基金会授予的10万美元,用于领导该项目,该项目将评估使用质子束治疗儿童脑瘤所导致的儿童发育障碍的风险。
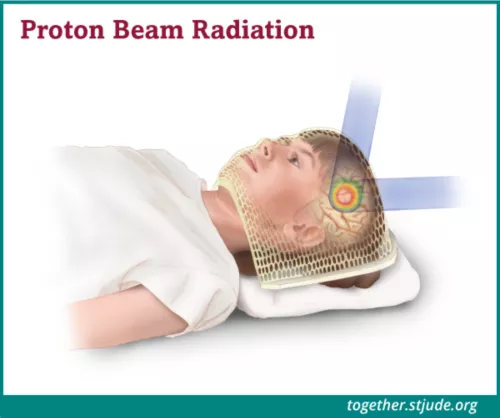
与传统的X射线(光子)疗法相比,质子束疗法能更好地瞄准肿瘤和癌细胞,向肿瘤提供最佳的辐射剂量,同时限制对周围健康组织的影响。
"Dell'Oro说:"在治疗儿童脑瘤时,这一点尤其重要,因为他们的大脑正处于敏感的发育阶段,极易受到影响。
质子的设计是为了使辐射更符合目标体积,既保护目标之前和之后的健康组织,也保护肿瘤周围的关键结构。
"Dell'Oro说:"我们知道质子治疗对患有脑瘤的儿童有较少的发育副作用,但我们需要更深入地研究,找出年龄、性别和个人对辐射的敏感性如何减轻或增加风险。
人们认为女性和年轻的病人对放疗更敏感,但现有的研究是基于成人的数据,而这些数据已经超过五年了--在一个快速发展的领域被认为已经过时了。
"放疗中使用的技术--包括质子束治疗和X射线--从那时起已经有了长足的进步,我们需要开发新的模型来预测儿童继发性原发性癌症和其他并发症的风险。"
南方大学的研究人员将使用来自田纳西州孟菲斯的圣裘德儿童研究医院的计算机断层扫描数据集,这是一个专门研究儿童癌症的儿科治疗和研究机构。这些数据将帮助当地研究人员建立一个数学模型来预测病人的结果。
脑瘤占所有儿童癌症的20%,占澳大利亚儿童癌症死亡人数的39%。他们的治疗方法包括手术、化疗和放疗,所有这些都与风险有关。
放疗会对儿童的神经系统、内分泌和认知能力造成一系列轻度至严重的负面影响。由于质子治疗更具针对性,它是儿童的首选治疗方法。
"从我们知道的情况来看,质子治疗的副作用不那么严重,生存结果也相似,但我们的知识仍有巨大差距。
"Dell'Oro说:"观察物理副作用需要数年时间,而且由于实际原因,临床试验很难进行,因此我们需要研究计算模型来估计患者的风险。
质子治疗中心的数量正在全球范围内迅速扩大,全世界有89个设施,主要集中在美国,但在欧洲和亚洲也有分布。
澳大利亚布拉格质子治疗和研究中心将是该国第一个质子治疗中心,位于北台地的南澳大利亚健康和医学研究所(SAHMRI)内。
预计该中心每年将治疗多达700名患者,其中约一半是儿童和年轻人。
在最近发表在《癌症》杂志上的一篇论文中,研究人员比较了三个年龄组的儿童患者的最新质子和光子辐射传输技术。与光子治疗(传统的X射线放射治疗)相比,质子治疗在所有情况下都减少了辐照量。
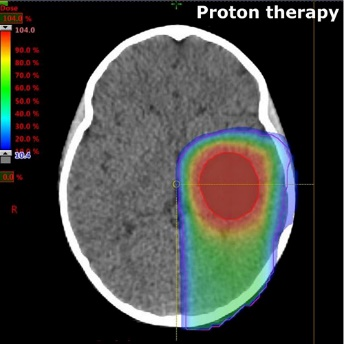
图1 质子治疗
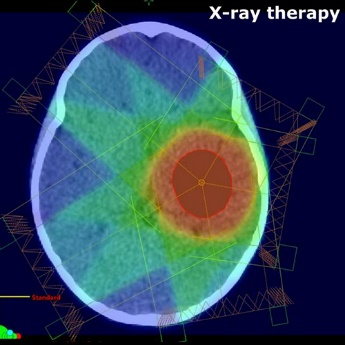
图2 X射线光子放疗
How safe is proton therapy for children with brain cancer compared to the conventional x-ray radiation delivered post-surgery?
A new study by University of South Australia (UniSA) researchers will explore this question over the next two years, using data from a US hospital to model patient outcomes based on individual cancers, radiosensitivity, sex and age of the children.
UniSA PhD candidate Mikaela Dell’Oro and her supervisors (Dr Michala Short, Dr Puthenparampil Wilson and Prof Eva Bezak) have been awarded $100,000 by the Channel 7 Children’s Research Foundation to lead the project, which will assess the risk of developmental disorders in children as a result of using proton beams to treat paediatric brain tumours.
Compared to conventional x-ray (photon) therapy, proton beam therapy superiorly targets tumours and cancer cells, delivering optimal radiation doses to the tumour while limiting the effects on the surrounding healthy tissues.
“This is particularly important when treating brain tumours in children because their brains are at a sensitive stage of development and highly susceptible,” says Dell’Oro.
Protons are designed to deposit radiation more conformally to the target volume, sparing both the healthy tissues before and beyond the target as well as critical structures surrounding the tumour.
“We know that proton therapy has fewer developmental side effects on children with brain tumours, but we need to dig deeper and find out how age, sex and an individual’s sensitivity to radiation also mitigate or increase the risk,” Dell’Oro says.
It is thought that females and younger patients are more sensitive to radiotherapy but existing research is based on adult data which is more than five years old – considered outdated in a rapidly advancing field.
“The techniques used in radiotherapy – both proton beam therapy and x-rays – have come a long way since then and we need to develop new modelling to predict the risk of secondary primary cancers and other complications in children.”
UniSA researchers will use computed tomography data sets from St Jude Children’s Research Hospital in Memphis, Tennessee, a paediatric treatment and research facility specialising in childhood cancers. This data will help local researchers build a mathematical model to predict patient outcomes.
Brain tumours comprise 20 per cent of all childhood cancers and account for the largest number of paediatric cancer deaths in Australia at 39 per cent. They are treated with a combination of surgery, chemotherapy and radiotherapy, all associated with risks.
Radiotherapy is responsible for a range of mild to severe neurologic, endocrine and cognitive negative effects in children. Because proton therapy is more targeted, it is the preferred treatment for children.
“From what we know, proton therapy has less severe side effects and similar survival outcomes, but there is still a huge gap in our knowledge.
“It takes years to observe physical side effects and clinical trials are difficult due to practical reasons, so we need to look at computational modelling to estimate the risks for patients,” Dell’Oro says.
The number of proton therapy centres is rapidly expanding around the globe, with 89 facilities worldwide, predominantly in the United States, but also in Europe and Asia.
The Australian Bragg Centre for Proton Therapy and Research will be the country’s first, located in the South Australian Health and Medical Research Institute (SAHMRI) on North Terrace.
It is anticipated the centre will treat up to 700 patients a year, with around half of these children and young adults.
In a paper recently published in the journal Cancers, the researchers compared the latest proton and photon radiation delivery techniques for paediatric patients across three age groups. Proton therapy reduced irradiation in all cases compared to photon therapy (conventional x-ray radiation therapy).
特别声明:以上内容(如有图片或视频亦包括在内)来自University of South Australia (UniSA),如有不实或侵权,请联系更正或删除。
免责声明:本网站文章内容仅作交流参考,不作为诊断及医疗依据,专业医学问题请咨询专业人士或专业医疗机构。
- 2023-04-18
- 2023-04-18
- 2023-04-18
- 2023-04-18
- 2023-04-18
- 2023-04-18
-
-
肝癌治疗队伍越来越庞大!数据显示:肝癌质子治疗后,70%患者肿瘤消失
医学上的肝癌,主要是指肝细胞癌。其他还有肝细胞癌、胆管细胞癌、肝转移癌等,不过俗称的肝癌,每年全球接近100
넶0 2023-04-18 -
-
-







